“Am I gonna make it, doc?”
The U.S. Centers for Disease Control website notes that the you are at risk for serious—even life-threatening—illness from Coronavirus if you are over age 60–65 or have a serious chronic medical condition, like…
- heart disease
- diabetes
- kidney disease
- lung disease
Well, there are at least a couple hundred heart diseases, a couple hundred kidney diseases, a couple hundred lung diseases, and at least three kinds of diabetes. There are entire thick medical textbooks written specifically for heart disease, lung disease, and kidney disease. All of those individual diseases don’t make you particularly vulnerable to Coronavirus.
And what’s a “serious condition?” Doctors don’t always tell you how serious a disorder is, and patients don’t always hear and remember when the doctor does. So you have a heart murmur. It’s likely chronic but is it serious? It depends.
I’ve even seen hypertension listed as a risk factor for serious flu complications, but I don’t believe it.
And what’s chronic? Say five years ago you had a mild heart attack, a stent was put in the only blocked artery, you take your prescribed drugs, and your doctor told you last month you’re doing great. Do you still have a serious chronic medical ailment?
By the way, physicians are calling the disease caused by Coronavirus “COVID-19.”
Is Age Really Important?
Yes. Here’s a chart from the report of UK’s Imperial College COVID-19 Response Team dated March 16, 2020:

Age-specific hospitalization and ICU admission rates from the Imperial College COVID-19 Response Team
TL;DR version: The need for hospitalization and ICU (intensive care unit) admission starts to rise dramatically for patients aged 50-59 and shoots up from there. If you make it into the ICU with COVID-19, you’ll quite likely have a tube down your throat and be on a ventilator (a mechanical “breathing machine”), or getting ECMO.
BTW, the Response Team figures you have only a 50:50 chance of surviving if you end up on a ventilator.
How Do I Know If I Have a Serious Chronic Medical Condition?
If you’re uncertain, the answer should come from your personal medical specialist or primary care physician. I know many of you will be unsure.
Here’s a simple test you can do to see if you might have a serious chronic medical condition:
- Walk up two flights of stairs without stopping
If you can’t do that without stopping to rest and without much shortness-of-breath (you should be able to carry on a conversation): you flunk. Possible explanations (among many) include serious heart or lung disease, being badly overweight, or just “out of shape” from lack of regular exercise. A couple of those conditions you can rectify, and should.

Artist’s rendition of Coronavirus (plus red blood cells, which in reality are orders of magnitude larger than viruses)
If You Have One of the Following Conditions, You Need to Be Extra Careful When Coronavirus Is Around
Having practiced medicine for over three decades—and I’ll keep practicing until I get it right—here’s my current list of conditions that raise your risk of serious disease if you contract Coronavirus:
- age over 60–65 (may not be much of a risk factor if you are otherwise healthy, physically fit, and eat well)
- needing supplemental oxygen at home, whether continuously, at night only, or just as needed
- moderate or severe valvular heart disease, whether the valve is leaky or blocked
- a weak heart muscle called cardiomyopathy with left ventricular ejection fraction under 50% or on home oxygen
- history of congestive heart failure with current left ventricular ejection fraction under 50% or on home oxygen
- moderate to severe diastolic heart failure (sometimes call “heart failure with preserved ejection fraction”)
- serious coronary artery disease (e.g., frequent chest pains, multiple heart attacks, residual blockages in arteries)
- asthma that requires daily drugs or that has frequent or severe exacerbations (the CDC says “moderate to sever asthma”)
- COPD (chronic obstructive pulmonary disease) or emphysema requiring daily scheduled drugs or frequent “as needed” drugs or home oxygen
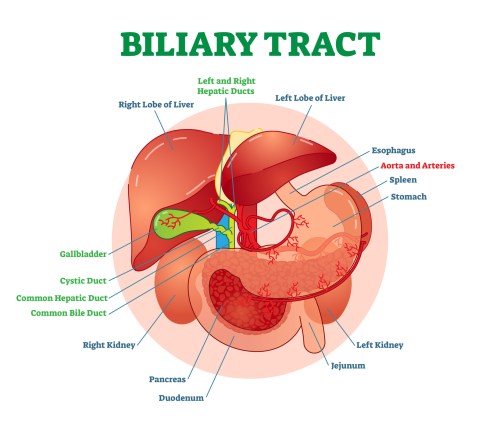
- chronic liver disease (such as cirrhosis) with serum bilirubin over 2.0 mg/dL or albumin under 3.0 g/dL or elevated prothrombin time
- serious active cancer, particularly if on chemotherapy that suppresses the immune system
- prior organ transplant requiring immunosuppressive drug therapy to prevent organ rejection
- immunoglobulin deficiency
- very sedentary lifestyle
- poor nutrition and/or malnutrition
- morbid obesity (CDC says severe obesity: body mass index 40 or greater)
- body mass index over 35
- on chronic corticosteroid therapy
- end-stage renal disease on dialysis
- chronic kidney disease with serum creatinine over 2 mg/dL
- nephrotic syndrome
- diabetes mellitus, especially if poorly controlled and/or concomittant chronic organ impairment such as nephropathy, neuropathy, or retinopathy
- active autoimmune disease (e.g., systemic lupus erythematosis, rheumatoid arthritis, Crohn’s disease), particularly if on drug therapy that impairs immune system function
- chronic low white blood cell count
- chronic active infection (e.g., tuberculosis, hepatitis, AIDS)
- smoker?
- you “always catch what’s going around” (possible immune system disorder or poor hygeine?)
Why Do These Conditions Increase Risk of Serious Illness?
Many of these infirmities impair your immune system and increase your risk of serious complications from any infection, whether viral, bacterial, or fungal. Just as importantly, these disorders may impair your body’s ability to respond to the increased physical stress of infection. Clearly, the more of these ailments you have, the greater your chance of a bad outcome.
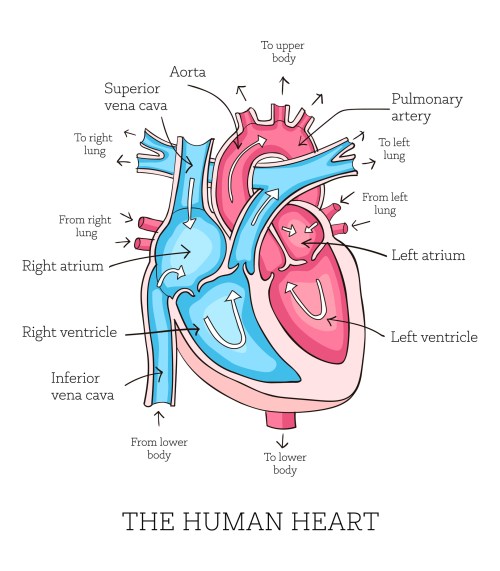
Here’s the problem when you come down with flu or any other infection. The infection increases the workload on various organ systems that keep you alive day in and day out. Even if you take an antibiotic or anti-viral drug, you still need various organ systems to keep you alive. I’m thinking particularly about your lungs, cardiovascular, and immune systems, working together at maximal capacity. You heart, for example, pumps about five liters of blood every minute while you’re at rest, blood that’s carrying life-preserving oxygen to all your other organs in addition to the heart muscle. That blood also carries a waste product—carbon dioxide—to your lungs for delivery to the outside world. If you exercise vigorously your heart increases it’s pumping output to twenty liters a minute, if you’re young and healthy. By the same token, your lungs have a certain but limited capacity to take up oxygen from the air and blow off carbon dioxide both at rest and during exercise. As we age, the capacity the heart and lungs to do their jobs diminishes no matter what. Same with the immune system. That’s why folks over 60 are at risk for serious complications from viral and other infections. Because infections increase the workload on the heart, lungs, and immune system. When Coronavirus infects your lungs, fluid and inflammatory debris builds up in the gas-exchanging tissues, impairing your ability to absorb oxygen from the air. So your lungs and heart have to work harder, and long enough for your immune system to eradicate there virus.
I hope you find this list more helpful than CDC’s. Nevertheless, I’m sure it’s incomplete. I’m not trying to scare you. I’m trying to help you survive the pandemic, as most of us will. Forewarned in forearmed.
If You Have One or More of the Listed Conditions, What Does “Being Extra Careful Around Coronavirus” Mean?
Avoid the virus if at all possible. The U.S. Centers for Disease Control and state governments have been issuing guidelines. One major issue is that the virus incubates in the body without symptoms for 5–7 days, and the affected individual may be infectious—shedding the virus that could get into you if you’re nearby—for 24 hours or so before the virus carrier even knows they’re sick. For folks that get sick with the virus, symptoms last for 1–2 weeks, and their oral or respiratory secretions (and feces? tears?) could infect you if the they enter your body via the mouth, nose, or eyes (or gastrointestinal tract?). Even after recovery, infected individuals can shed infectious virus for about a week. Further complicating the situation is that infected individuals may just have mild symptoms like a cough (or runny nose or sneezing?), and won’t be quarantining themselves or avoiding other people. They won’t know they have the virus. Other people can harbor the virus in their bodies and never feel sick—we don’t know how infectious these folks are. So what specifically can you do if you have risk factors for serious disease?
- Monitor your local news reports to know how common is the virus in your community. If there’s an outbreak there or where your’e going…
- Avoid crowds (0f 10 people? 50?)
- Stay home as much as possible.
- Don’t be around people with symptoms of possible COVID-19: c0ugh, shortness of breath, fever, ?sneezing, ?runny nose. Sure, they could just have common illnesses like bronchitis, pneumonia, hay fever, allergies, the common cold, or a sinus infection. You just don’t know. The virus won’t get into your residence unless you allow an infected person in.
- Avoid touching high-touch surfaces in public places, like hand rails, elevator buttons, door handles, handshakes, etc. If you must touch, cover the surface with a tissue or disinfect it first.
- Wash your hands frequently with soap and water. Particularly after touching high-touch surfaces in public places.
- Avoid cruises, mass transit, air travel. Again: crowds.
- If you can’t avoid someone who’s coughing or sneezing, offer them a surgical mask.
- Don’t touch your mouth, nose, or eyes. That’s how germs on your hands can enter you.
Steve Parker, M.D.
PS: It’s still very early in this pandemic and there’s much we don’t know. Some of the above information is probably wrong. Stay tuned.
Updated on March 30, 2020, after reading this from the CDC. (I wonder if someone there read my post.) If memory serves, the original CDC fact sheet listed hypertension as a risk factor for serious illness, but that’s gone now.

Click the pic to purchase at Amazon.com. E-book versions also available at Smashwords. com.