This is from the cited journal article. I hope this is considered fair use rather than copyright infringement.
This is the most creative therapeutic approach to Alzheimer’s Disease I’ve seen in a while. It may even be preventative. I have no idea whether it will pan out in the long run. I’m always skeptical.
Abstract
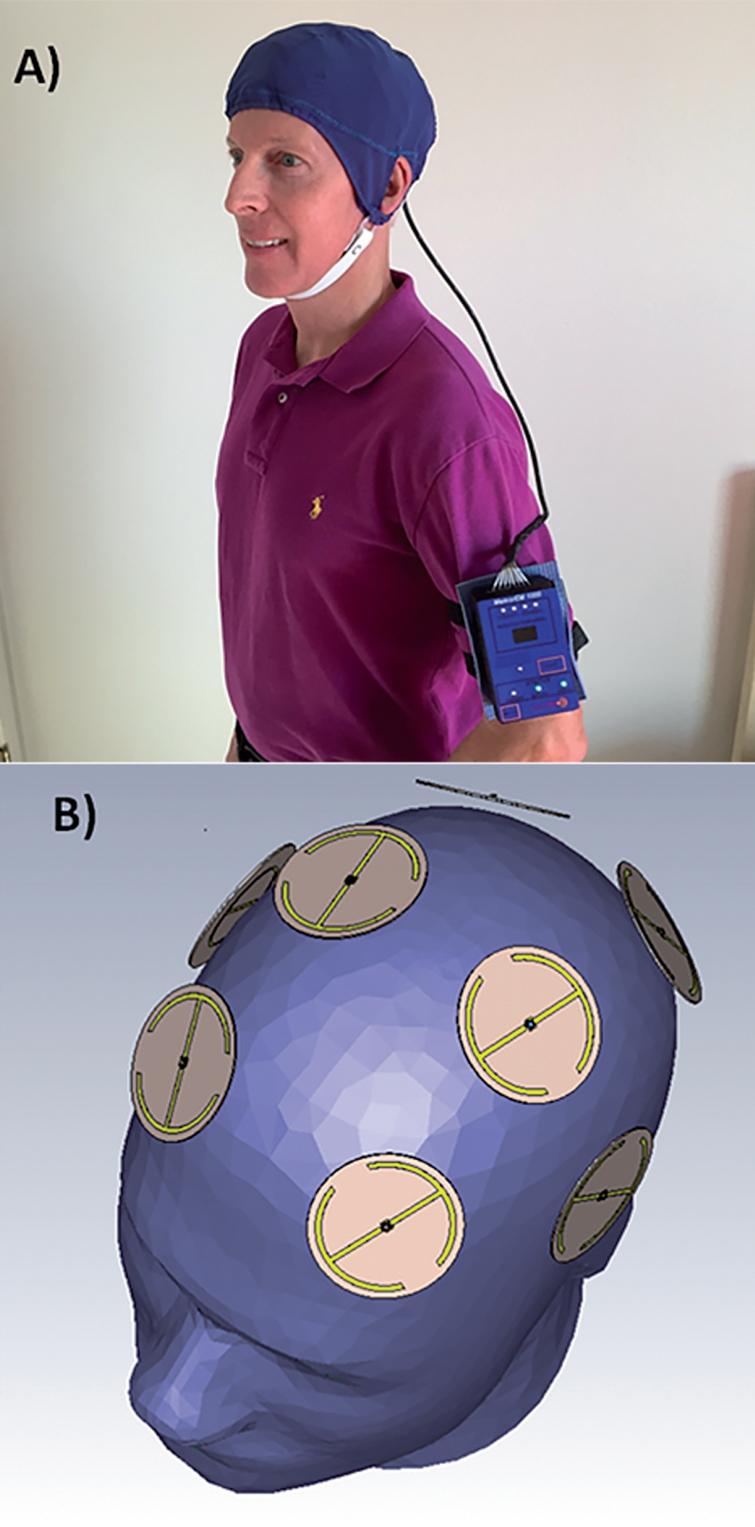
Background: Small aggregates (oligomers) of the toxic proteins amyloid-β (Aβ) and phospho-tau (p-tau) are essential contributors to Alzheimer’s disease (AD). In mouse models for AD or human AD brain extracts, Transcranial Electromagnetic Treatment (TEMT) disaggregates both Aβ and p-tau oligomers, and induces brain mitochondrial enhancement. These apparent “disease-modifying” actions of TEMT both prevent and reverse memory impairment in AD transgenic mice.
Objective: To evaluate the safety and initial clinical efficacy of TEMT against AD, a comprehensive open-label clinical trial was performed.
Methods: Eight mild/moderate AD patients were treated with TEMT in-home by their caregivers for 2 months utilizing a unique head device. TEMT was given for two 1-hour periods each day, with subjects primarily evaluated at baseline, end-of-treatment, and 2 weeks following treatment completion.
Results: No deleterious behavioral effects, discomfort, or physiologic changes resulted from 2 months of TEMT, as well as no evidence of tumor or microhemorrhage induction. TEMT induced clinically important and statistically significant improvements in ADAS-cog, as well as in the Rey AVLT. TEMT also produced increases in cerebrospinal fluid (CSF) levels of soluble Aβ1-40 and Aβ1-42, cognition-related changes in CSF oligomeric Aβ, a decreased CSF p-tau/Aβ1-42 ratio, and reduced levels of oligomeric Aβ in plasma. Pre- versus post-treatment FDG-PET brain scans revealed stable cerebral glucose utilization, with several subjects exhibiting enhanced glucose utilization. Evaluation of diffusion tensor imaging (fractional anisotropy) scans in individual subjects provided support for TEMT-induced increases in functional connectivity within the cognitively-important cingulate cortex/cingulum.
Conclusion: TEMT administration to AD subjects appears to be safe, while providing cognitive enhancement, changes to CSF/blood AD markers, and evidence of stable/enhanced brain connectivity.
Steve Parker, M.D.
PS: I notice that several of the study authors are based in my area of operations, south-central Arizona.
PPS: The Mediterranean diet for years has been linked to lower risk of dementia.