“I’ll practice extreme social distancing even after house-arrest is lifted for others.”
BREAKING NEWS: Gray hair is a risk factor for serious COVID-19 infection.
I keep reading that hypertension (high blood pressure) makes one vulnerable to COVID-19. For instance, many patients hospitalized in New York had hypertension. The implication is that something about hypertension weakens your immune system such that you’re more likely to die.
In the study linked above, average age of all hospitalized was 63. Fifty-seven percent of them had hypertension. Most healthcare providers know that the prevalence of hypertension rises with age. So you’d expect lots of 63-year-olds to have hypertension. At least 25% of them, right?
With just ten seconds of googling, I found that the prevalence of hypertension in the U.S. for those 60 and older is 63%. I fully expect my blood pressure would be higher than it is now if I lived in New York City, which I’ll never do.
If you’re 63-years-old and hospitalized in New York City for anything, odds are you’re likely to have hypertension. Just like you’re more likely to have gray hair than someone younger. Hypertension and gray hair are incidental markers for advancing age. They don’t per se increase your risk of serious illness from COVID-19.
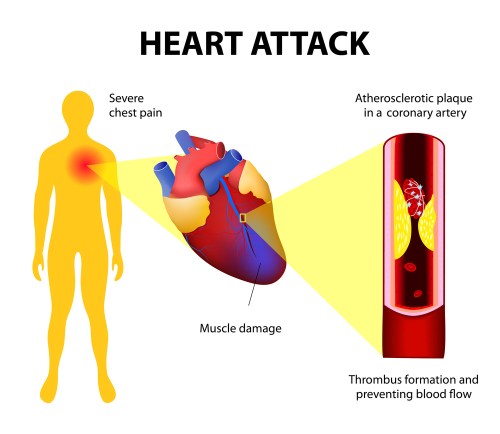
Now, that being said, be aware that uncontrolled hypertension can damage some major organs that are important for health and longevity. That’s why we treat it. That damage can weaken your heart, kidneys, arteries, and brain. You need those systems to help you fight off any serious infection, not just COVID-19. If you already have organ damage from uncontrolled hypertension, I’ll bet that increases your chances of a bad outcome from any serious infection. Regarding hypertension and function of the immune system, I’m not aware of any good data or connection.
My first link above was to a JAMA Network article detailing the co-morbidities of over 5,000 New York City area residents hospitalized with COVID-19. A few other data points from it:
- 42% were obese. What’s the obesity rate for 63-year-olds in New York City? I don’t know. Among all adults in New York state, the prevalence of obesity is 28%. This is about 3 points lower than the national average.
- 34% had diabetes. The study authors don’t make it easy to find, but I bet this is mostly type 2 diabetes. I don’t know the prevalence of diabetes in New York City. In the U.S. overall, among those 65 or older, the prevalence of diabetes is 27%. I’d say at least 90% of that is type 2 diabetes. That 27% includes the 5% who don’t know they have it.
- Mortality rates for those who received mechanical ventilation in the 18-to-65 and older-than-65 age groups were 76.4% and 97.2%, respectively. Those mortality rates are scary high, but let’s not put too much emphasis on them yet since some of these folks were still in the hospital at the time the report was prepared.

Tracheal intubation in prep for mechanical ventilation
Bottom Line
If I were a 30-years-old and had well-controlled hypertension or gray hair, I wouldn’t worry much about my risk of COVID-19. On the other hand, if I were obese, I’d work on fixing that, starting NOW. Regarding diabetes, if you can’t cure it, keep it under control.
Steve Parker, M.D.
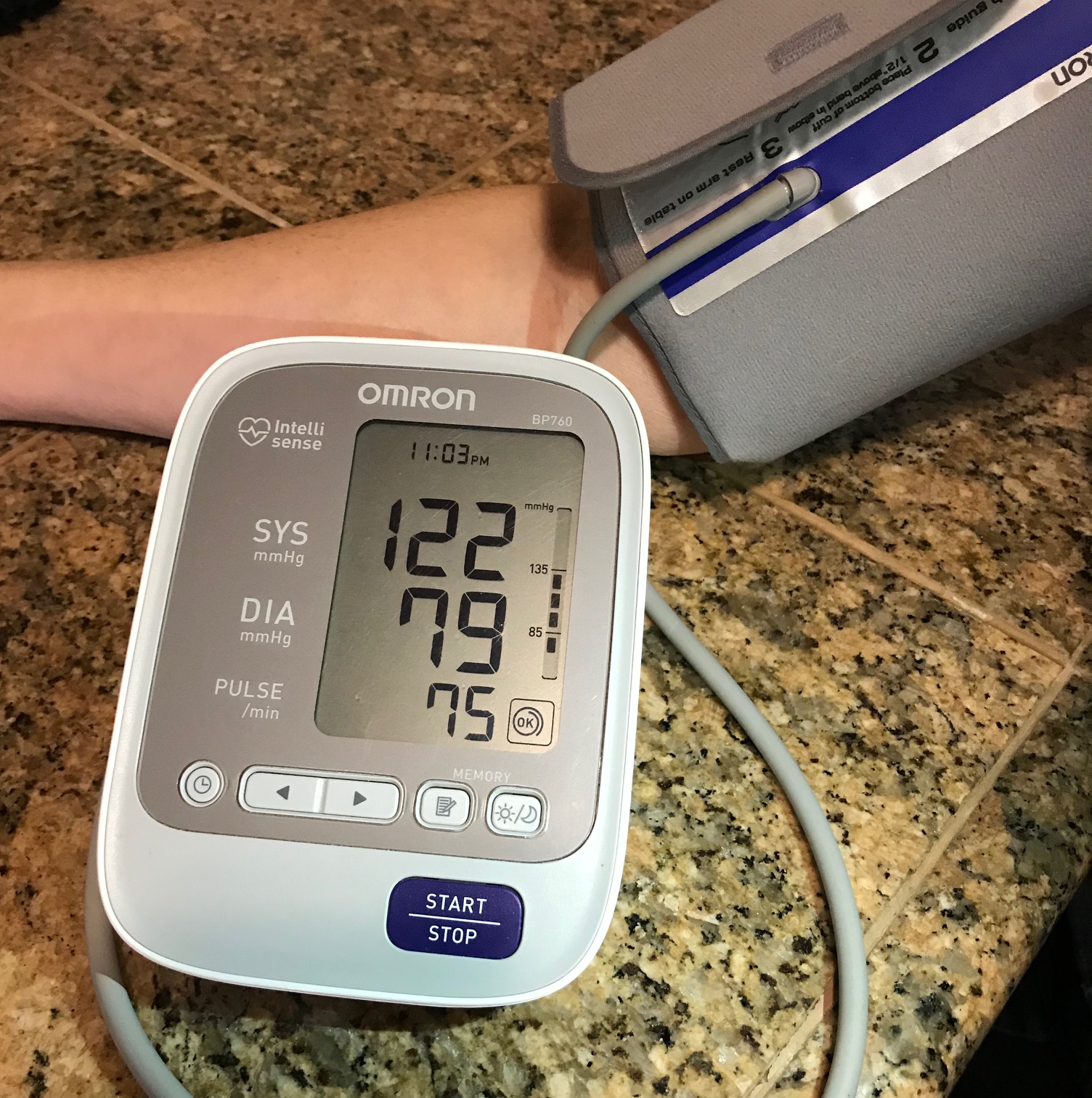
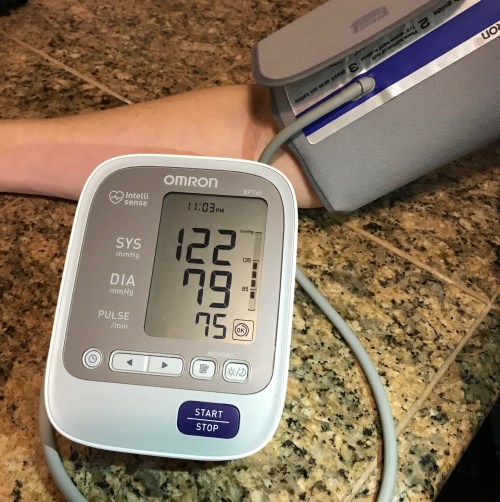
PS: Did you know the definition of hypertension changes over time? Even the one below is outdated. The linked CDC report above used this definition:
Hypertension: Systolic blood pressure greater than or equal to 140 mmHg or diastolic blood pressure greater than or equal to 90 mmHg, or currently taking medication to lower high blood pressure.
PPS: Admittedly, “60 and older” includes 93-year-olds. You may argue that the incidence of hypertension among 93-year-olds is 85% compared to 45% in 60-70 year-olds. Please do the research and show your work. I’m out of time.
PPPS: Overall prevalence of hypertension in the U.S. is 29%. Curious about the incidence of hypertension in other U.S. age groups?
- age group 18-39: 7.5%
- age 40-59: 33.2%
- 60 and over: 63.1%

Click the pic to purchase at Amazon.com. E-book versions also available at Smashwords. com.
Click pic to purchase at Amazon.com. E-book versions also available at Smashwords. com.