Here’s an excerpt from the recent Danish study that questions the efficacy of facemarks in preventing transmission of SARS-CoV-2 virus. Note that there were ~3,000 folks in both the experimental and control groups. The experimental group wore surgical masks, so this study says nothing about cloth masks, N95s, or bandanas. Also note this study was done at at time early in the pandemic when mask-wearing by the public was not at all common, quite a bit different from today’s world in many places. The investigators suggest that for face masks to prevent transmission of the virus, the masks need to be worn by already-infected, viral-shedding people.
In this community-based, randomized controlled trial conducted in a setting where mask wearing was uncommon and was not among other recommended public health measures related to COVID-19, a recommendation to wear a surgical mask when outside the home among others did not reduce, at conventional levels of statistical significance, incident SARS-CoV-2 infection compared with no mask recommendation. We designed the study to detect a reduction in infection rate from 2% to 1%. Although no statistically significant difference in SARS-CoV-2 incidence was observed, the 95% CIs are compatible with a possible 46% reduction to 23% increase in infection among mask wearers. These findings do offer evidence about the degree of protection mask wearers can anticipate in a setting where others are not wearing masks and where other public health measures, including social distancing, are in effect. The findings, however, should not be used to conclude that a recommendation for everyone to wear masks in the community would not be effective in reducing SARS-CoV-2 infections, because the trial did not test the role of masks in source control of SARS-CoV-2 infection. During the study period, authorities did not recommend face mask use outside hospital settings and mask use was rare in community settings. This means that study participants’ exposure was overwhelmingly to persons not wearing masks.
Steve Parker, M.D.
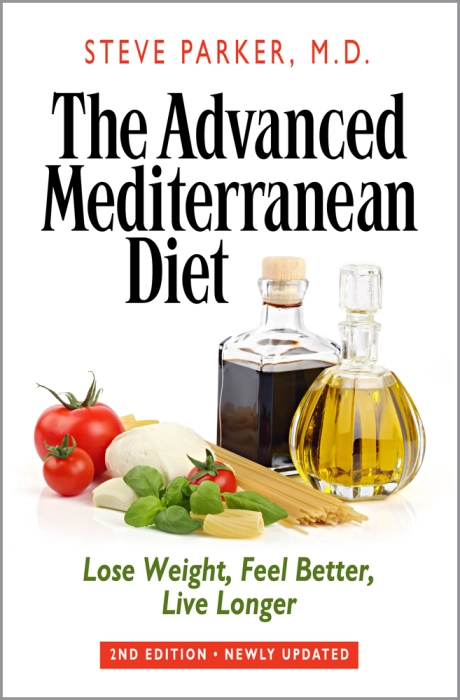
Click to purchase at Amazon.com. E-book also available at Smashwords. com.