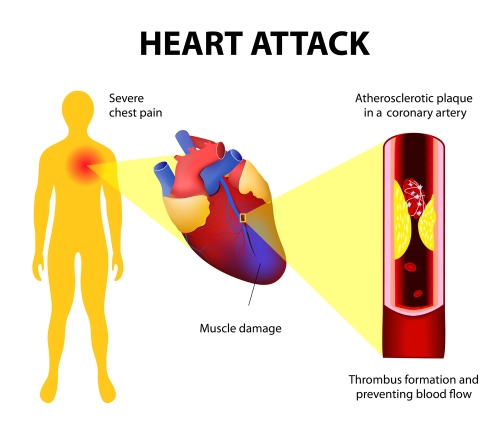
Most patients with a heart attack have underlying atherosclerosis (“hardening of the arteries”) in the heart, called coronary artery disease. Around the time of a heart attack (if not before), doctors and patients should focus on mitigating risk factors for future heart attacks and other cardiac events. This is called “secondary prevention.” Risk factor modification might include smoking cessation, regular exercise, stress reduction, and diet modification. For years, I’ve been recommending the Mediterranean diet. Many others recommend a low-fat diet instead. A recent study supports my diet recommendation.
One way to assess risk of progressive atherosclerosis is to measure the thickness of the the carotid artery wall by ultrasound. Increasing thickness of the artery wall is linked to higher risk of atherosclerotic complications like heart attack and stroke. To drill down deeper, it’s the thickness of the innermost two layers of the artery wall, called the intima-media, that matters. The study at hand showed a reduction in carotid artery intima-media thickness over five years on a Mediterranean diet compared to a low-fat diet. Here’s the abstract:
Background and Purpose:
Lifestyle and diet affect cardiovascular risk, although there is currently no consensus about the best dietary model for the secondary prevention of cardiovascular disease. The CORDIOPREV study (Coronary Diet Intervention With Olive Oil and Cardiovascular Prevention) is an ongoing prospective, randomized, single-blind, controlled trial in 1002 coronary heart disease patients, whose primary objective is to compare the effect of 2 healthy dietary patterns (low-fat rich in complex carbohydrates versus Mediterranean diet rich in extra virgin olive oil) on the incidence of cardiovascular events. Here, we report the results of one secondary outcome of the CORDIOPREV study. Thus, to evaluate the efficacy of these diets in reducing cardiovascular disease risk. Intima-media thickness of both common carotid arteries (IMT-CC) was ultrasonically assessed bilaterally. IMT-CC is a validated surrogate for the status and future cardiovascular disease risk.
Methods:
From the total participants, 939 completed IMT-CC evaluation at baseline and were randomized to follow a Mediterranean diet (35% fat, 22% monounsaturated fatty acids, <50% carbohydrates) or a low-fat diet (28% fat, 12% monounsaturated fatty acids, >55% carbohydrates) with IMT-CC measurements at 5 and 7 years. We also analyzed the carotid plaque number and height.
Results:
The Mediterranean diet decreased IMT-CC at 5 years (−0.027±0.008 mm; P<0.001), maintained at 7 years (−0.031±0.008 mm; P<0.001), compared to baseline. The low-fat diet did not modify IMT-CC. IMT-CC and carotid plaquemax height were higher decreased after the Mediterranean diet, compared to the low-fat diet, throughout follow-up. Baseline IMT-CC had the strongest association with the changes in IMT-CC after the dietary intervention.
Conclusions:
Long-term consumption of a Mediterranean diet rich in extravirgin olive oil, if compared to a low-fat diet, was associated with decreased atherosclerosis progression, as shown by reduced IMT-CC and carotid plaque height. These findings reinforce the clinical benefits of the Mediterranean diet in the context of secondary cardiovascular prevention.
Parker here again. Undoubtedly, it would be more helpful if the investigators reported the actual rates of heart attack, stroke, and death in the two diet groups over five years. I suspect that will be in a future report.
An article in Clinical Cardiology states the serious nature of coronary artery disease (CAD) in those with diabetes (DM): “CAD is the main cause of death in both type 1 and type 2 DM, and DM is associated with a 2 to 4-fold increased mortality risk from heart disease. Over 70% of people >65 years of age with DM will die from some form of heart disease or stroke. Furthermore, in patients with DM there is an increased mortality after MI [myocardial infarction], and worse overall long-term prognosis with CAD.”
Steve Parker, M.D.


Click to purchase at Amazon.com. E-book also available at Smashwords. com.


